In a surprising turn of events, Central Florida has become an unexpected hotspot for leprosy, a rare and ancient disease that has perplexed the medical community for centuries. Dr. Rajiv Nathoo, a dermatologist in Orlando, was taken aback when he diagnosed a 54-year-old landscaper with the condition, as the patient lacked the typical risk factors associated with the infection.
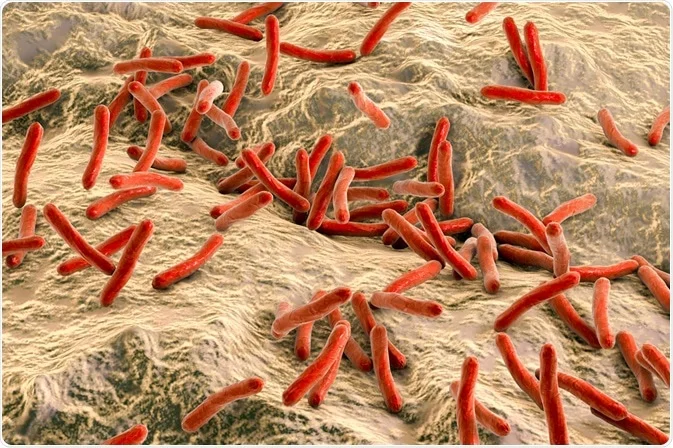
Leprosy, also known as Hansen’s disease, is caused by the bacteria Mycobacterium leprae, which attacks nerves under the skin, leading to telltale symptoms like numb or insensitive lesions and rashes. Traditionally, most cases in the United States were linked to travel to countries with high leprosy rates or exposure to armadillos, which can carry the disease. However, a cluster of cases in Central Florida suggests a more complex transmission pattern.
Researchers have discovered that approximately 34% of new cases between 2015 and 2020 lacked the typical risk factors, indicating that leprosy may have become endemic in the region. While experts agree that leprosy is becoming more common in the area, there is no need for public health panic, as the overall numbers remain relatively low.
One of the challenges with leprosy is its slow incubation period, which can take up to 20 years before symptoms manifest. This delayed onset makes it difficult to track the source and spread of the infection, and often results in misdiagnoses. Dr. Charles Dunn, a study author and chief resident at Advanced Dermatology and Cosmetic Surgery Clinics, stresses the importance of dispelling misconceptions about the disease, as not all cases can be traced back to armadillos or foreign travel.

Left untreated, leprosy can lead to severe consequences, including paralysis, blindness, and irreversible nerve and skin damage. Fortunately, the infection is curable with a combination of antibiotics taken over a few years. However, for those whose diagnosis is delayed, the cure may not fully reverse the damage already done.
Healthcare providers in the area are now being cautioned to be vigilant for similar cases, as early diagnosis is crucial in preventing further transmission. Patients often go for months without a correct diagnosis, as leprosy is not commonly seen in the United States. Dr. Linda Adams, chief of the laboratory research branch at the National Hansen’s Disease Program, emphasizes the need for increased awareness among medical professionals.
While the origin of the leprosy cluster in Central Florida remains unclear, it serves as a stark reminder that diseases can emerge unexpectedly in new areas. Understanding the transmission patterns of leprosy is essential to curb its spread and protect public health. As the medical community continues to investigate this puzzling outbreak, it is crucial for healthcare providers across the nation to remain vigilant for potential cases and expand their knowledge on this rare and enigmatic disease.